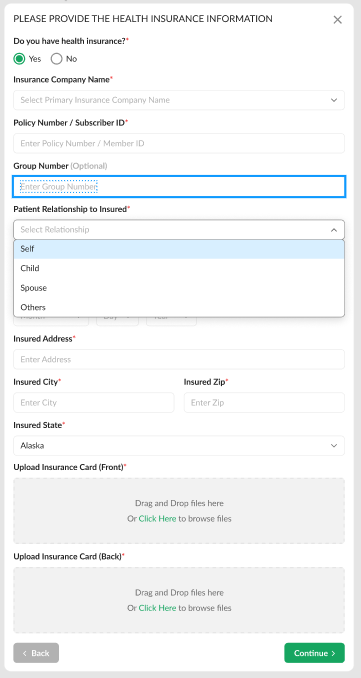
As a Patient, you can now choose to let your health insurance pay for you (or your dependents') telemedicine consultation with your VSee Provider.
Note: This feature may not be available in your clinic. Please contact Sales or your Account Manager to enable this feature.
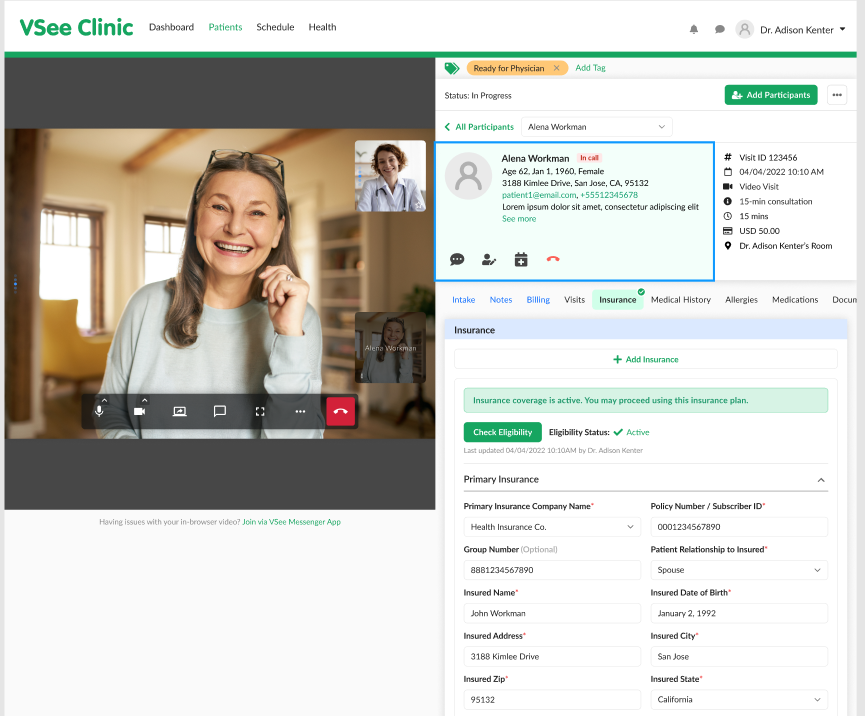
As a Provider, you can check and add the Patient’s eligibility information during the visit.
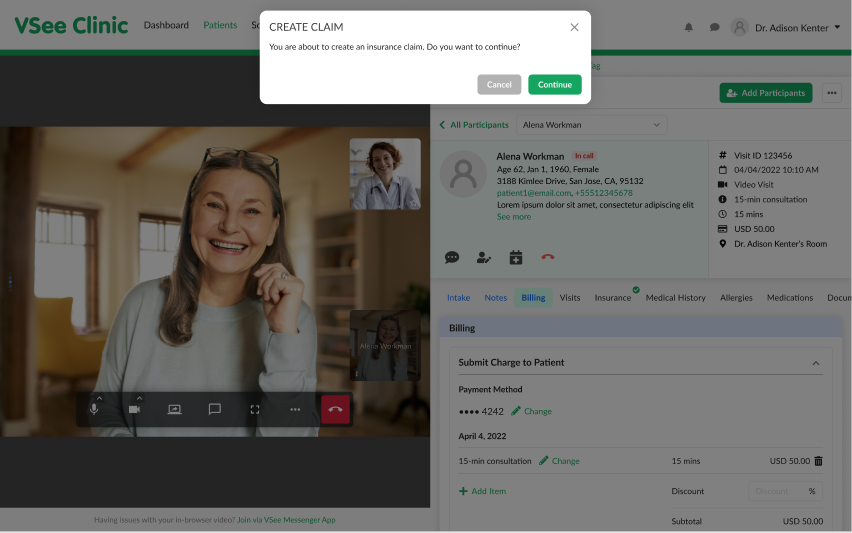
You can even submit a medical claim so that the Patient’s health insurance can pay for your services to the Patient or the Patient’s family members.
To learn more, read through these articles:
Scope and Limitations:
An insurance claim can only be created using an insurance plan with an “Active” status.
Currently unable to view claim status via VSee Clinic / Patient Portal.
Currently, Procedure and Diagnosis details are not reflected on the invoice.
An insurance plan with an “Active” eligibility status cannot be edited or removed by the patient until the eligibility period has expired. Or if the provider chooses to update it themselves on their end.
Two is the maximum number of insurance plans a patient may add per patient account. If ever the primary insurance plan is removed, the secondary insurance plan will become the primary.
Currently, the Diagnosis and Procedure codes will only be added to the insurance claim form after the Provider has clicked the “Sign & Send” button.
If you have any questions, please contact us at help@vsee.com.
Last updated on: 15 July 2022
